In 1997 UCSF epidemiologist and Brain Tumor Center researcher Margaret Wrensch, PhD, first identified a curious link between the virus that causes chickenpox and decreased risk of glioma.
With funding from a new National Institutes of Health (NIH) Research Project grant, Stephen Francis, PhD, an associate professor in the Department of Neurological Surgery, wants to figure out the genetic factors at the root of this association.
Francis and his research group are interested in how the genetics underlying the immune response to common viruses correlates with glioma risk and survival. These studies could help scientists better understand which genetic factors cause these brain tumors.
“To our knowledge, there’s no other cancer like this,” Francis said, emphasizing that scientists still don’t have a good explanation for the association between prior chickenpox infection and glioma.
Francis and his colleagues are using information from Bay Area Adult Glioma study. This UCSF study that Wrensch, a professor in the Department of Neurological Surgery, started in 1991 contains clinical and epidemiologic data from over 1,000 people with glioma and 1,000 individuals of the same age, sex, and race without cancer.
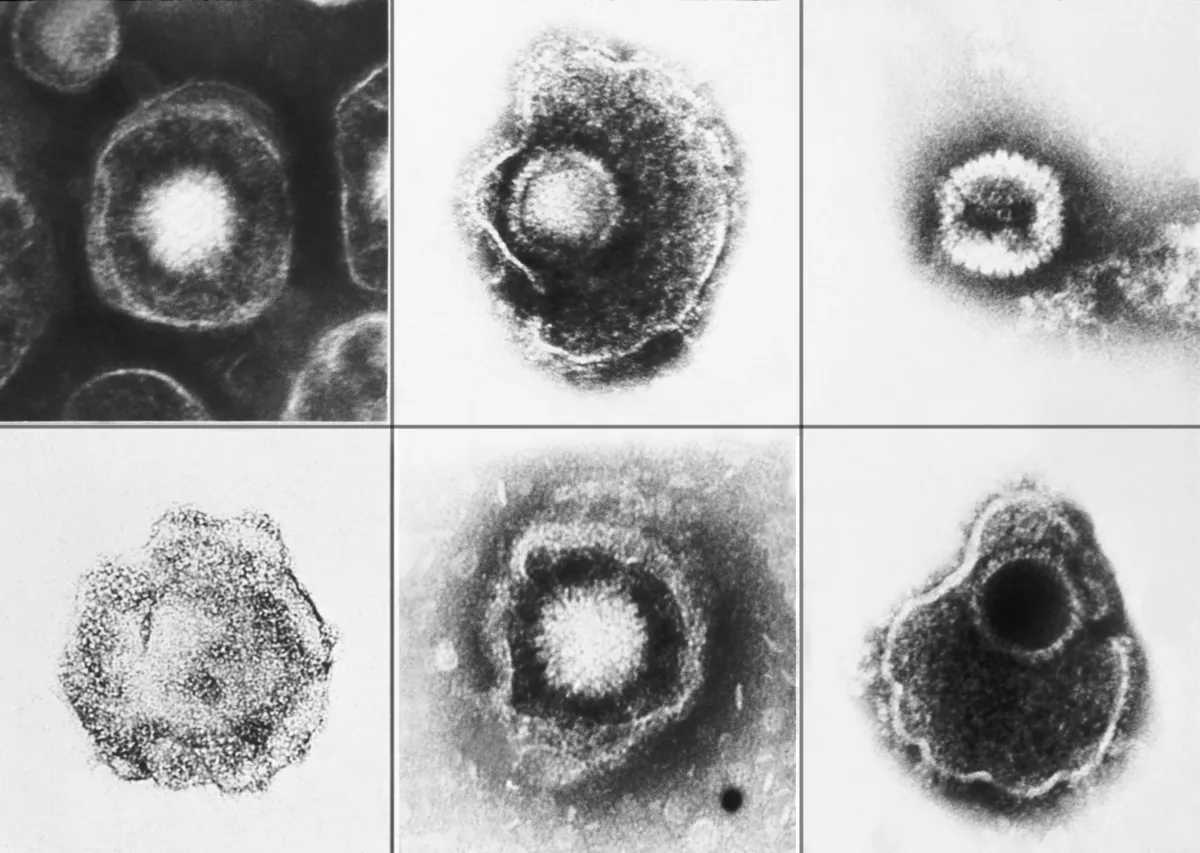
The Francis group can now examine the inherited genetic programming that influences the immune response to different viral antigens. In some preliminary studies, they have found that the magnitude of immunological reactivity to varicella zoster virus — a herpesvirus that causes chickenpox and shingles — is associated with how long a person with glioma might expect to live once diagnosed with a brain tumor.
Using a technique called phage display, Francis says that the scientists can also screen antigens for different common viruses to get a clear picture of how glioma risk correlates with each. Since all herpesviruses are similar, he’s interested in seeing if the others evoke an analogous response. These experiments will also allow the researchers to test whether the association is specific to certain parts of the varicella zoster virus.
Independent of the viruses, the Francis lab is focusing on the region of the human genome where the human leukocyte antigen (HLA) genes regulating the immune system are located.
Single nucleotide polymorphisms (SNPs) are DNA variants at a single base position in the genome, and scientists often use genome-wide association studies (GWAS) to detect SNPs that are more common in people with a given disease. However, Francis explains that these studies don’t necessarily identify the exact variants that contribute to disease. Instead, GWAS might flag other variants within that genomic region that are inherited together.
Since HLA has the most diversity of any region in the human genome, Francis says scientists have struggled distinguishing those associated with disease.
With targeted deep sequencing of the HLA region, Francis says he and his colleagues would be able to pinpoint if any HLA polymorphisms influence the risk of getting glioma and the survival trajectory once diagnosed.
In the last piece of their study, the Francis lab will assess whether specific polymorphisms within HLA that are associated with the glioma risk interact with certain viruses. This analysis will allow them to check if these are independent risk factors for glioma.
Francis hopes their systematic approach will guide scientists developing targeted therapeutics to improve glioma survival outcomes. His lab’s findings, for example, could suggest that existing anti-herpesvirus medications or the live attenuated shingles vaccine would provide potential survival benefits in some glioma patients.
The data from individuals without glioma, Francis says, will also help scientists learn more about how humans react to viruses and how inherited germline mutations might alter that relationship.
“These are really difficult long-term things to study that really can only be done at the population-level,” Francis said.
