Glioma is an aggressive brain cancer that often grows back after initial treatment, but many research models study the disease in tumors that have never received any therapies.
Aaron Diaz, PhD, an associate professor in the Department of Neurological Surgery at UC San Francisco, is studying the differences between these tumors at initial diagnosis versus recurrence. With new funding from an National Institutes of Health (NIH) Research Project grant, Diaz hopes his lab’s research could uncover new treatments to better manage the disease.
UCSF has one of the largest and most comprehensive brain-tumor programs in the U.S. Consequently, the UCSF Brain Tumor Center has an extensive archive of biospecimens available to researchers, like Diaz, through the Neurosurgery Biorepository.
“We have this really unique opportunity to leverage this cohort and try to understand, for the first time, the effect of standard therapy on the cellular composition of gliomas,” Diaz said.
Scientists have often conceptualized tumor evolution as how new mutations might give some cells within a tumor the competitive advantage to keep growing — and perhaps even avoid therapies.
Under the Glioblastoma Precision Medicine Program, Diaz and his colleagues compared paired tissue samples from glioblastoma patients before and after receiving treatment with temozolomide and ionizing radiation.
The researchers found that the genetics of the glioblastoma cells weren’t evolving in response to therapy. This work, Diaz said, corroborates other studies indicating that the genetic evolution of gliomas occurs early in the transition from a normal brain cell into a cancerous cell.
The tumor cells instead adopt a treatment-resistant response called the mesenchymal state. As part of this adaptive response, the cells change their metabolism and their physical shape to evade the anticancer therapies. Then, following treatment, they transition back to being fast-growing.

The Diaz lab is now investigating how to predict these different cellular states. “Understanding the different cell state transitions that these tumor cells undergo to avoid therapy will allow us to derive combination therapies that can cut off these escape routes,” Diaz said.
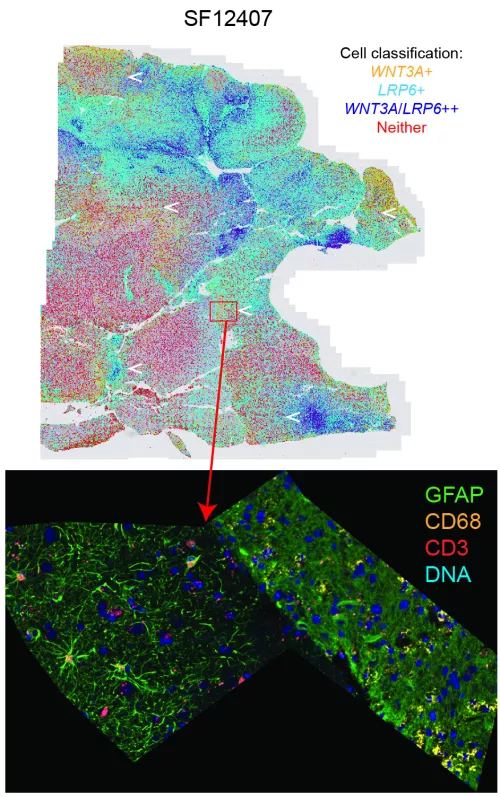
The scientists characterize how tumor cells behave and quantify gene expression levels. With new advances in RNA measurements, the researchers can see where all the genes of cell are located across a tissue slice.
Diaz’s team is focusing on understanding how some glioma cells can repair the DNA damage that ionizing radiation causes. These studies, according to Diaz, could drive the development of adjuvant chemotherapies that could be given together with radiation therapy to make it more effective.
Diaz wants to figure out if existing drugs could be repurposed to treat glioma. His lab has recently been looking at published analyses and databases of known drug-gene interactions.
Based on their preliminary bioinformatics analysis, the researchers have identified some antipsychotic medications as potential drug targets. Although these drugs weren't originally developed to treat brain cancers, they can affect cellular processes that indirectly affect the pathways tumor cells would need to repair DNA damage.
Because antipsychotics can cross the blood-brain barrier, Diaz says these medications would already be past a big hurdle facing new candidate treatments.
While many recurrent gliomas have the same DNA mutations, some tumors acquire many new mutations in response to treatment with temozolomide. Scientists think that tumors with more mutations may respond better to immunotherapies, so Diaz’s research group also wants to predict which patients are more likely to develop these hypermutated tumors.
As the Diaz lab continues studying the changes that gliomas undergo at recurrence, the group is marking some transitions of their own. Karin Shamardani and Francisca Catalan both recently started graduate school while Lin Wang and Husam Babikir moved on to academic and industry positions, respectively.
And Diaz — now a midcareer faculty member — wants to keep helping the next generation of trainees succeed.
