The immune landscape in glioblastoma differs from other types of cancers, rendering current immune checkpoint blockade ineffective at treating this malignant brain tumor.
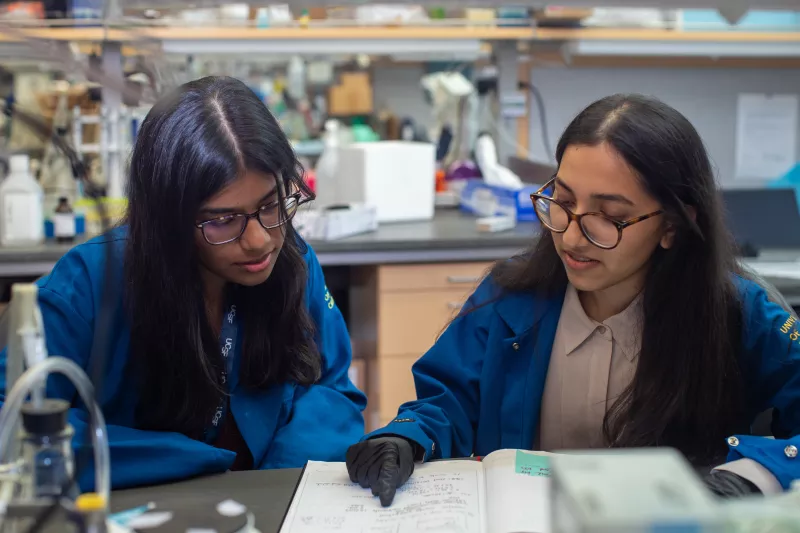
New UC San Francisco faculty member Rongze “Olivia” Lu, PhD, an assistant professor in the Department of Neurological Surgery, studies the tumor microenvironment in glioblastoma. She hopes to improve immunotherapy by reprogramming cells within the tumor generate more antitumor inflammatory signaling molecules.
Lu’s studies focus on macrophages and microglia, two types of cells that make up nearly half the tumor mass. These cells interact with the cancer cells and modulate the surrounding immune environment.
Lu describes microglia and macrophages as having “flexible” signaling responses within tumors. The cancer cells often direct them to promote cell growth and mediate immune suppression. For example, these cells can stop T cells from killing the brain tumor cells.
However, a district group of macrophages and microglia can help the T cells to kill cancer cells by producing an anti-inflammatory cytokine called Type I interferon. This cell population exists in low frequency within glioblastoma.
Lu and her colleagues have found that inhibiting an enzyme called protein phosphatase 2A (PP2A) in macrophages and microglia makes them produce more Type I interferon and helps T cells battle the tumor cells.
In preclinical mouse models, Lu’s research group also showed that immune checkpoint inhibitors work better against glioblastoma when treated with a small molecule inhibiting PP2A. This discovery introduces a new strategy to fight these brain tumors and may benefit many patients with this horrible disease.
Now, with funding from a new National Institutes of Health (NIH) Research Project grant, Lu’s lab is examining the underlying mechanisms how PP2A inhibition enhances Type I interferon in macrophage and microglia, with the goal to develop novel immunotherapy for glioblastoma.
“We have multiple lines of research demonstrating PP2A is a very promising target for brain tumor therapy to enhance the immune response in the brain tumor microenvironment,” Lu said. “We will work on developing novel drug candidates to target PP2A through collaboration at UCSF.
Lu, who recently moved from the University of Texas at Austin, is excited to foster collaborations with her new research and clinical colleagues in the UCSF Brain Tumor Center, Helen Diller Comprehensive Cancer Center, and larger campus. She draws inspiration from the passion her fellow researchers have for finding innovative treatments for brain tumor patients.
And her background as a scientist in the pharmaceutical industry drives her keep pushing to get scientific discoveries from the bench into drug development and clinical trials.
