Immunotherapy has improved outcomes for many cancer patients, but unfortunately, aggressive brain cancers like glioblastoma do not respond to this treatment.
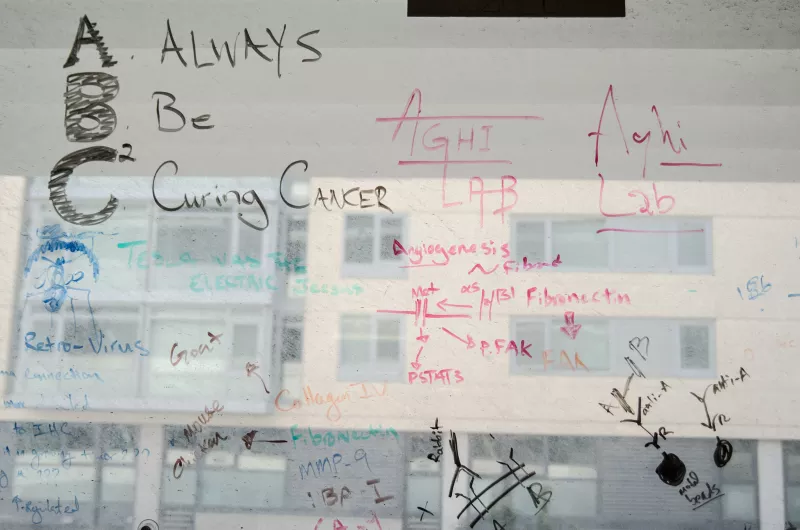
Scientists think that the immune system is not properly working in glioblastoma cells, so some UCSF Brain Tumor Center researchers are studying how to ramp up the immune response. New funding from a National Institutes of Health (NIH) Research Project grant is helping Manish Aghi, MD, PhD, a professor in the Department of Neurological Surgery, develop new gene therapy approaches for treating the disease.

Cancer gene therapy refers to the strategy of using a virus to infect a tumor. Scientists have typically generated replicating viruses that can kill the cancer cells themselves or viruses that transport a gene toxic to the cancer cells. But more recently, Aghi says that researchers have shifted towards trying to make viruses that can both spread and deliver other kinds of genes.
In a previous clinical trial, Aghi and his colleagues used a replicating retrovirus developed by his collaborator Noriyuki Kasahara, MD, PhD to deliver a gene that activated a chemotherapy drug. Although this trial didn’t yield positive results, the scientists now have new insights to overcome the prior study’s limitations.
“One of the things that's come out of that interpreting that trial as well as others,” Aghi said, “has been the recognition that these viruses are really immune therapies, and they stimulate an immune response.”
Now, Aghi and Alex Haddad, MD, a second-year neurosurgery resident in Aghi’s lab, are using gene therapy to get pro-inflammatory molecules to the tumor. Their leading candidate is RLI, a molecule that enhances the immune signaling activity of the cytokine IL-15.

Aghi says his lab has seen encouraging preliminary results with RLI in mouse models of glioblastoma. “We were getting 10 to 20 percent cure rates in a model that's really aggressive, and 100 percent cure rates in a model that's slightly less aggressive,” he said.
These findings in preclinical experiments corroborate observations from the last clinical trial that suggested a subset of patients might be more likely to benefit from this type of therapy.
“We saw examples of very robust inflammatory reactions that were favorable, but these responses only developed if the patient had four cycles of the drug,” Aghi said, noting that slower-growing malignant tumors may afford doctors a therapeutic window for treating the disease.
With the goal of eventually getting this therapy into patients, Aghi’s research group is now studying how to make RLI more effective. For example, the researchers want to combine RLI with systemic immunotherapies used in other cancers, like immune checkpoint inhibitors, to see if that additive effect makes the therapy even more potent.
Aghi and his colleagues are also interested in seeing whether the therapy stimulates enough immunologic memory, which helps the immune system prevail in repeat confrontations against the tumors cells. Preclinical fast-growing tumor models generated less immune memory, suggesting the RLI gene therapy may work better if the virus supplies other cytokines as well.
Additionally, the scientists want to see if treating tumor cells with RLI plus the drug from the previous trial would evoke a better immune response. “That virus went into hundreds of patients, and we don't want to just discard it because it failed,” Aghi said. “We want to try and strengthen it.”
For Aghi, who worked on viruses when he was an MD PhD student, these studies are a return to his roots as a scientist but with the benefit of more than ten years of experience studying the basic biology of glioblastoma.
