For 4th grader Gio Perry, December 3, 2019 began as a normal school day in his small hometown of Palm Coast, Florida. But on the bus ride home, he developed a massive headache.
“I was waiting for him at the bus stop,” said Gio’s mother Cera. “I saw him stumble off the bus and fall to the ground. He was unresponsive, with foam at the mouth and eyes rolled back as my husband picked him up.”
A CT scan in the emergency room revealed bleeding in the brain that resulted from the rupture of an arteriovenous malformation (AVM) – an abnormal tangle of arteries and veins. AVMs in children are extremely rare, representing only 3% of the 3,000 AVM cases diagnosed every year, although they tend to rupture more frequently than in adults.


Gio was helicoptered to a children’s hospital in Orlando, where he remained connected to an intracranial pressure monitor, external ventricular drain, feeding tube, and breathing tube.
“It was terrible,” Cera said, as she watched Gio in a coma-like state and doctors suggested waiting for his AVM to heal before attempting treatment. “When you’re faced with this emergency, and your child is experiencing a life-threatening condition, you just want to follow what the doctor recommends.”
As Gio slowly began to recover, he spent another month at an inpatient rehabilitation facility to regain his ability to walk and speak, and the Perrys began to research surgical treatment options that would prevent the AVM from re-rupturing.
Gio’s AVM was located in the posterior fossa near the brainstem – a particularly delicate area of the brain to operate on. If the AVM bleeds during surgery, it can lead to significant neurological impairment.
Despite consultations with several local physicians, the Perrys were unable to find a surgeon with the expertise to perform the surgery, and with the added burden of the COVID-19 pandemic, they experienced extensive delays for the neuroimaging they needed to make critical decisions. “There was nothing but negativity on his condition,” said Cera.
With options waning, Cera got in touch with the Aneurysm and AVM Foundation, a non-profit patient advocacy group that connected her to the Pediatric Brain Center at UCSF. Within a week of receiving Gio’s angiogram (an x-ray of the blood vessels) vascular neurosurgeon Adib Abla, MD, called Cera to tell her that he and the team felt that Gio was a good candidate for surgery.

"Gio's AVM was complex and sitting partially within the brainstem and middle cerebellar peduncle. Given the location and the rarity of lesions in this critically sensitive location, several surgeons had told the family to consider radiosurgery as the risks of surgery were felt to be high," Abla said.
"However, when the family reached out, I immediately realized that a cure was possible and would be obtained right away with surgery. Given the number of AVMs I had treated in the same location, I reassured the family that I had complete confidence in our center's ability to tackle this AVM with surgery."
“It was a relief that was lifted off my shoulders,” recalled Cera. “After many setbacks, Dr. Abla called me personally, answered all my questions, and was very transparent about any risks. He made me feel comfortable and that he cared.”
The PBC’s neurosurgery program sees a higher number of similar AVM cases that might be considered inoperable elsewhere. “We’re not just a referring center for Northern California. As leaders in vascular surgery, we see patients from all over the country and care for the most challenging cases that are best suited for a high-volume center with a lot of experience,” said Abla.
The multidisciplinary team of pediatric specialists involved in Gio’s care also included pediatric neurosurgeons Nalin Gupta, MD, PhD and Peter Sun, MD, and neurointerventional radiologist Van Halbach, MD.
Beyond an experienced team, the advanced surgical technology available at UCSF also played a part in the Perry’s decision to travel to UCSF for Gio’s treatment. “Another reason why I chose UCSF was the intraoperative angiogram,” Cera continued.
In UCSF’s state-of-the-art hybrid-angiography operating suite, Dr. Abla and his team can obtain high-quality angiograms in the operating room, allowing them to assess the brain’s blood flow and make any adjustments, as needed. Previously, patients would undergo a second procedure for the angiogram and, if needed, schedule another surgery for revisions. The Perry family was relieved that the availability of intraoperative angiography meant fewer procedures for Gio.
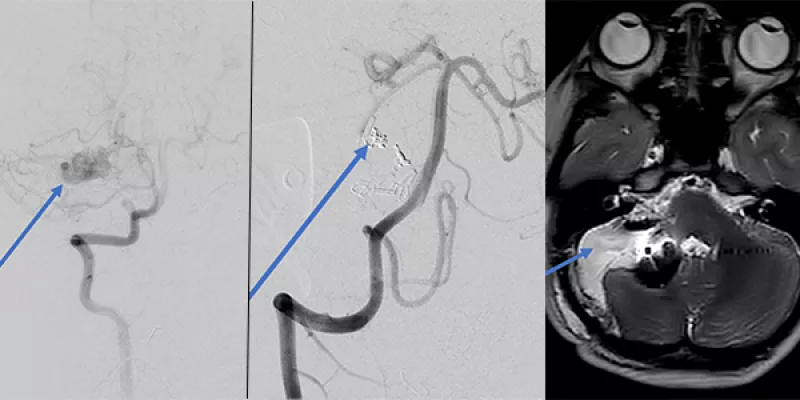
"The intraoperative angiogram has been another game changer for our patients. The surgery went exactly as planned and the AVM was removed in its entirety, which we verified that same day before we closed [the skull]," Abla said.
The Perry family flew back to Florida four days after surgery, reuniting with Gio’s four other siblings. Four months after surgery, Gio is an active fifth grader who loves trampoline jumping and video games. “It wouldn’t have happened if we didn’t come to UCSF. It was because of Dr. Abla’s expertise,” said Cera.


