The models many hospitals use to predict the outcomes of patients with traumatic brain injury (TBI) may need to be revised, according to a recent study from researchers at UC San Francisco, UC San Diego, and other U.S. institutions.
The International Mission on Prognosis and Analysis of Clinical Trials in Traumatic Brain Injury (IMPACT) and Corticosteroid Randomization After Head Injury (CRASH) prognostic models for TBI were created from data collected between 1984 and 2004 and do not factor in advances in TBI medicine over the last 20 years.
In the new study, researchers tested whether outcomes predicted by the IMPACT and CRASH models correlated with observed patient outcomes from a more modern dataset: the Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI) study. TRACK-TBI prospectively enrolled patients at 18 U.S. Level 1 trauma centers from 2014-2018. Their analysis in 831 patients revealed that overall, fewer people with TBI were dying than predicted.
The new findings, recently published in the Journal of Neurosurgery, show how the IMPACT and CRASH models may not be as applicable to certain TBI patients in the modern era, especially subgroups of older patients or patients with moderate TBI.
“Care has evolved, and our understanding of TBI has evolved,” said Geoffrey T. Manley, MD, PhD, Professor and Vice Chair of Neurosurgery at UCSF, Chief of Neurotrauma at Zuckerberg San Francisco General Hospital and Trauma Center, and the study’s co-senior author.
Towards better assessments of TBI
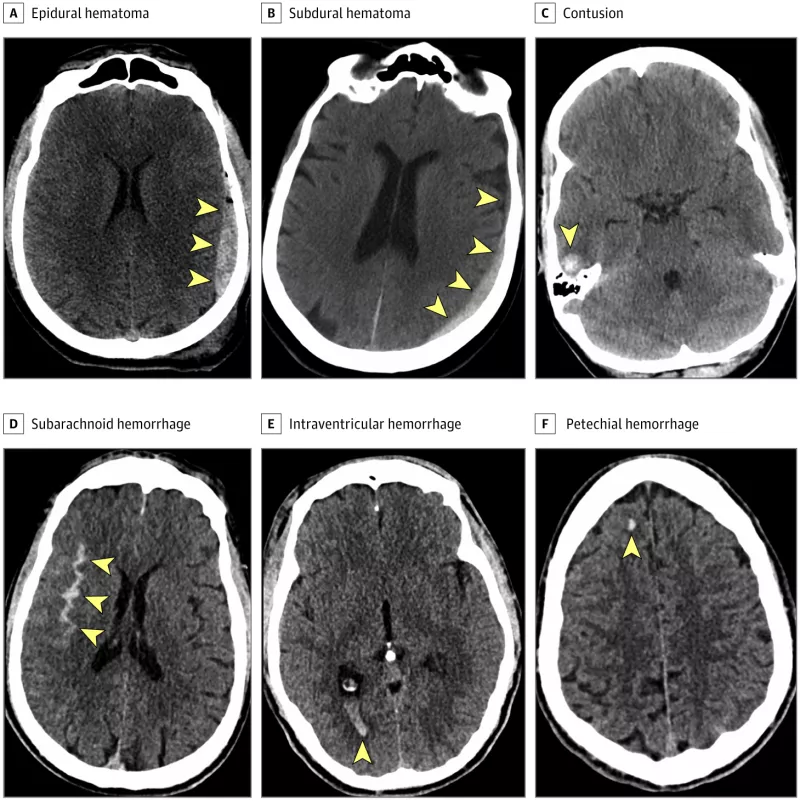
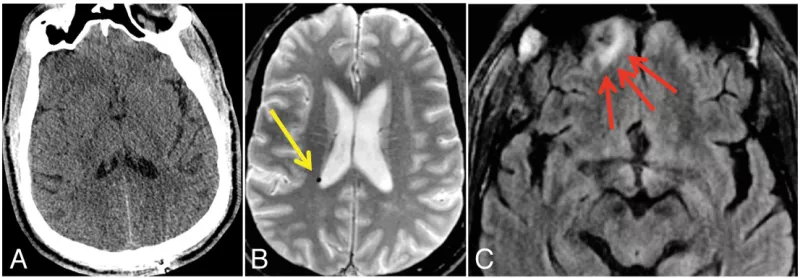
Part of the reason for the discrepancy between predicted versus real-world outcomes is that TBI represents a broad group of patients, says study co-first author and sixth-year UCSF Neurosurgery resident John K. Yue, MD. In the emergency setting, physicians use the Glasgow Coma Scale (GCS) score to identify disruptions to consciousness and evaluate TBI severity. As a combined metric of a patient’s eye, verbal, and motor responses, injuries to different regions of the brain can end up with the same GCS score despite disparate component responses.
Since both the IMPACT and CRASH models use components of GCS scores, they inherit these limitations in their assessment of TBI. “These are not the most accurately calibrated models for patients with moderate TBI due to the higher injury heterogeneity inherent in the moderate TBI group,” Yue said. “We need to be more careful when making statements about this group of patients.”
The scientists similarly found that the models were not accurately forecasting outcomes for patients over 65. “Even though these models account for age, we need more sensitive approaches to move towards more personalized predictors for patients in the modern era,” Yue said.
For example, TRACK-TBI researchers have already shown that the concentrations of the proteins GFAP and UCH-L1 found in the blood after TBI can be used to diagnose intracranial injuries not visible on CT scans and predict death and severe disability at six months. These studies helped lay the groundwork for the U.S. Food and Drug Administration’s recent clearance of a blood test including these biomarkers to assist in the clinical assessment of acute TBI at the bedside. In older patients, frailty may also be another important factor to integrate into prognostic models.
Yue also stresses that the CRASH and IMPACT models are just estimates informed by a single timepoint in a patient’s clinical history — the assessment made when they first arrive to the emergency department. Future prediction models should integrate data on diagnostics, progression and interventions.
Improving recovery for TBI patients
Importantly, Yue, Manley, and their colleagues underscored that TBI prognostic models are imperfect estimations of outcomes based on large aggregated datasets to guide injury classification and clinical decision-making. The models do not represent the ground truth for the future outcome of a patient in the acute care setting, nor should they be used in isolation to direct clinical care or counseling, they said.
An individual’s recovery depends on their overall health, which part of their brain was injured, and their access to rehabilitative care.
Other TRACK-TBI research shows that patients’ symptoms can still improve one year and beyond after their initial injury. Medical follow-up care and social support, Yue says, can further aid in TBI recovery. “Certainly, TBI refers to the acute injury, however in the recovery phase it becomes more similar to an acquired chronic condition,” he said.
To provide more integrated care for TBI patients, UCSF recently opened the Neurorecovery Clinic at the Weill Institute of Neurosciences at Mission Bay. The Neurorecovery Clinic offers patients referrals to neurosurgery and neurology clinicians, physical therapists, speech therapists, and occupational therapists who can help patients manage their symptoms.
“Outcomes are no longer static in TBI,” Yue said. “People continue to get better and that portends more hope in the current era.”
Watch our latest Community Grand Rounds to learn more about our neurotrauma team's approach to managing TBI.
Reference
Yue JK, Lee YM, Sun X, van Essen TA, Elguindy MM, Belton PJ, Pisică D, Mikolic A, Deng H, Kanter JH, McCrea MA, Bodien YG, Satris GG, Wong JC, Ambati VS, Grandhi R, Puccio AM, Mukherjee P, Valadka AB, Tarapore PE, Huang MC, DiGiorgio AM, Markowitz AJ, Yuh EL, Okonkwo DO, Steyerberg EW, Lingsma HF, Menon DK, Maas AIR, Jain S, Manley GT; The TRACK-TBI Investigators. Performance of the IMPACT and CRASH prognostic models for traumatic brain injury in a contemporary multicenter cohort: a TRACK-TBI study. J Neurosurg. 2024 Mar 15:1-13. doi: 10.3171/2023.11.JNS231425.
