About
Hello! My name is Roberto Rodriguez Rubio. I am a neurosurgeon trained in Guadalajara, Mexico and I am currently an assistant professor in the Department of Neurosurgery at the University of California, San Francisco (UCSF). Since the summer of 2017, I have been directing UCSF’s Skull Base and Cerebrovascular Laboratory (SBCVL), where our research is focused on pushing the boundaries of neurosurgical innovation and creating new models of sharing and teaching neuroanatomy.
3D Models in Neurosurgery
As neurosurgeons, our field is concerned with the diagnosis, surgical treatment, and rehabilitation of disorders affecting or implicating the nervous system. A neurosurgeon has to navigate through extremely delicate three-dimensional anatomy and to manipulate ever-changing variables in real-time. Such procedures require a high degree of familiarity with the visuospatial architecture of the relevant anatomy, and as such, necessitates years of training.
Historically, such training relied solely on dissections of cadavers and review of 2D anatomical illustrations and photographs. But given the inherent costs and shortages in cadaveric specimens, and the inability of 2D images to convey spatial relations, there has been a growing trend in the field to find new ways to depict neuroanatomy in 3D.
Today, a developing method for accomplishing this task is the creation of volumetric models (VM’s)—3D anatomical models which are frequently built from DICOM (Digital Imaging and Communications in Medicine) images, the standard format for handling medical imaging like that generated by CT or MRI scans. Although these DICOM-reconstructed models can help us better visualize the 3D orientation of different anatomical structures, they currently lack sufficient resolution and textures. These major drawbacks require time-consuming post-processing to get an accurate replica of anatomical features.
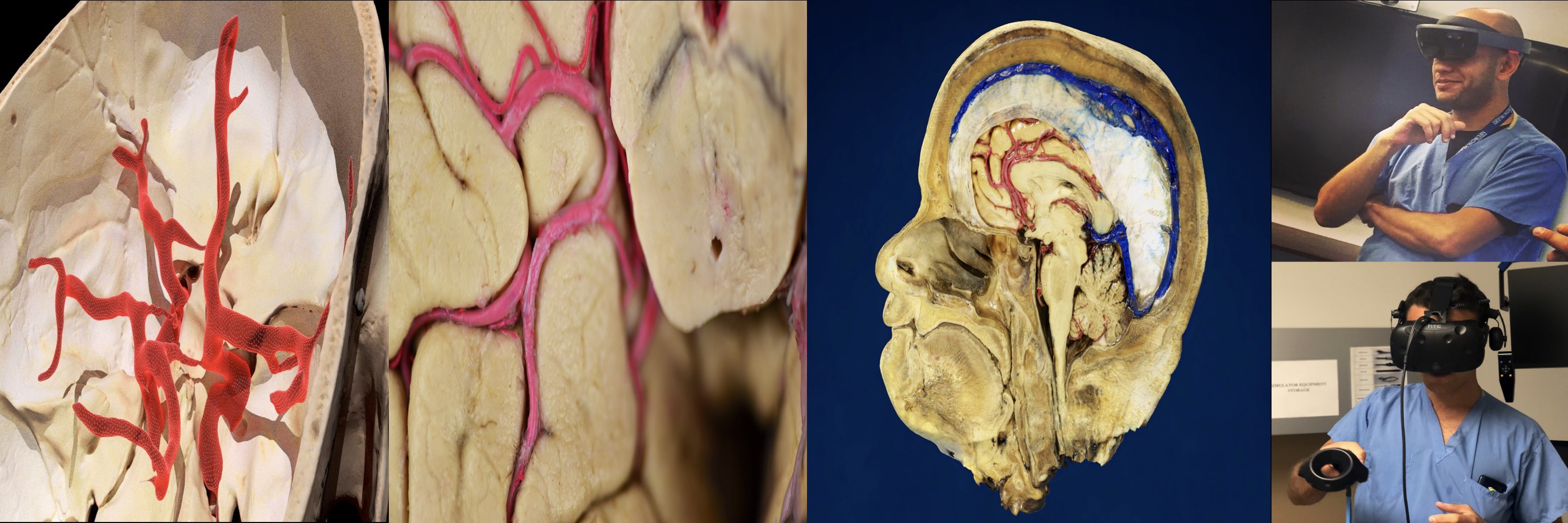
For these reasons, our laboratory uses commercially available three-dimensional scanning techniques to develop VMs from cadaveric surgical and anatomical dissections. These VMs are now part of our workflow to record and analyze anatomical pieces to provide a thorough view of the surgical neuroanatomy, precisely as it is seen by our team members at the SBCVL (Model 1).
Workflow
We first develop a dissection plan that includes the structures and surgical steps to highlight and the basic stereoscopic photographs or videos to take while exploring the anatomy. Then our team utilizes two popular techniques for capturing the desired anatomy: 1) Structured light scanning (SLS) using a portable 3D scanner (Figure 1) and 2) Photogrammetry (PGM) using a professional camera or an endoscopic camera (Video 1). Fundamentally, both techniques involve the capture of the specimen’s surface from various angles/elevations followed by post-processing, which reconstructs the obtained data into a 3D model. We opt to use SLS for most of the reconstructions in which small, tubular structures, such as nerves or vessels, and small openings in the skull, called foramina, are involved (Model 2). On the other hand, we tend to use PGM mostly for deep corridors, such as the nasal passages, and small structures, such as the inner ear bones, in which endoscopic cameras or macro lenses can allow us to get a better reconstruction of the anatomical features (Model 3).
Following additional aesthetic modifications and edits of meshes and textures, the resultant models are saved in our library and used to create stereoscopic animations (Video 2) and images (Figure 2) that serve as supplementary material to the standard stereoscopic photos included in the 3D neuroanatomy lectures we give every month to neurosurgery residents (Fig 3).
Finally, the models are uploaded to Sketchfab, prepared with relevant annotations, and tested with our VR headsets to be ultimately incorporated into scientific publications. The use of an online 3D viewer such as Sketchfab has facilitated us to share the models with students, residents, and neurosurgeons inside and outside our institution allowing them to explore the VMs without the need of going to an anatomy lab. (Fig 4) We have found that the best way to explore our anatomical VMs on Sketchfab is by using a VR headset. We often scale up the VMs so that the users can explore the models as if they were inside a house; the students are free to tour the model by following annotations or by identifying structures during live quizzes after one of our 3D lectures. It provides excellent supplementary didactic material that gives us the chance to conceptualize and explore the anatomy with students in a way that was not previously possible. One of our most popular models for VR use is a skull that we scanned using SLS (Model 4), please feel free to try it out and let us know if you enjoyed the experience.
- Figure 2.
- Figure 3.
- Figure 4.
*Readers with institutional access who may be interested in a more detailed description of the above workflow may find the following informative:
- Construction of Neuroanatomical Volumetric Models Using 3-Dimensional Scanning Techniques: Technical Note and Applications
- Acquisition of Volumetric Models of Skull Base Anatomy Using Endoscopic Endonasal Approaches: 3D Scanning of Deep Corridors Via Photogrammetry
The Future
As 3D image-capture technology continues to evolve, so will the fidelity and overall quality of the resulting VMs. Additionally, the interaction of these models with other 3D platforms may open the door to new levels of immersion in surgical simulation.
We recently published the first in a series of open-access articles that will include a collection of stereoscopic media and VMs with the aim of providing comprehensive immersive content to facilitate a better understanding of neurosurgical anatomy which is accessible to everyone. We hope that this series of articles will inspire more researchers and journal editors to use VMs as part of sharing their scientific work which, in turn, will facilitate further advances in the medical field.
The ultimate digital-to-physical translation of VMs that may prove to be the most revolutionary is 3D printing. Many medical fields, including orthopedics and radiology, regularly utilize 3D printing to complement clinical practice, and application of this technique to neurosurgical aims is something we are actively pursuing in our laboratory (Figure 5). Moreover, other modalities such as augmented reality and light-field displays will also allow us to portray 3D models that can be instantly visualized in 3D by colleagues and patients within their physical, real-world environments (Figure 6).
Most importantly, the primary goal of these efforts remains the improvement of our ability to treat and care for our patients. It is a humbling opportunity to play a role in the development of such budding technologies. VMs models are a great tool to teach, learn, and understand 3D anatomy, and thanks to this platform, everyone can interact with them. The next step will be to use the VMs for active virtual dissections and surgical simulations (i.e., removal of a tumor, aneurysm clipping) with realistic haptic-feedback and as an integration of image-guided systems for intraoperative neuronavigation.
Acknowledgments
We want to express our gratitude to the body donors and their families, who, through their altruism, contributed to making our 3D projects possible.
The author is also grateful to Todd Dubnicoff for critically reviewing this post.
Sketchfab Collections: Brain / Pterional / Endoscopic
Website / Instagram / UCSF Surgical Neuroanatomy Collection / Email Skull Base