
UCSF’s Ezequiel (Eze) Goldschmidt, MD, PhD, is a neurosurgeon specializing in minimally invasive techniques, including the endoscopic endonasal approach (EEA), to remove skull base and pituitary tumors.
“The endoscope provides a beautiful perspective of the surgical field and allows us to see, in detailed magnification, every aspect of the operation,” Goldschmidt said. “We can operate on most of the ventral skull base through an endonasal approach.”
The following case studies describe how Goldschmidt and the UCSF Brain Tumor Center team used the EEA to successfully remove different types of tumors, including a pituitary adenoma, a craniopharyngioma, an epidermoid cyst and a chondrosarcoma.
Patient’s vision restored after removal of pituitary adenoma
A 58-year-old man presented with severe vision loss. The MRI revealed a large sellar mass, which was diagnosed as a pituitary adenoma.
“The endoscope allowed us to see the entire extension of the tumor,” Goldschmidt said. “We first removed the calcified parts, then dissected the tumor from the cavernous sinus and removed it completely to decompress the optic chiasm.”
The patient’s vision returned to normal after the surgery, and a postoperative MRI showed complete removal of the lesion.
“Pituitary adenomas are relatively common,” Goldschmidt said. “We have removed many of them using the endonasal approach.”
The following cases illustrate how the UCSF team used the EEA for complex pathology.
Patient’s symptoms relieved after craniopharyngioma resection
A 38-year-old woman presented with progressive headaches, extreme fatigue, intermittent blurry vision and nausea.
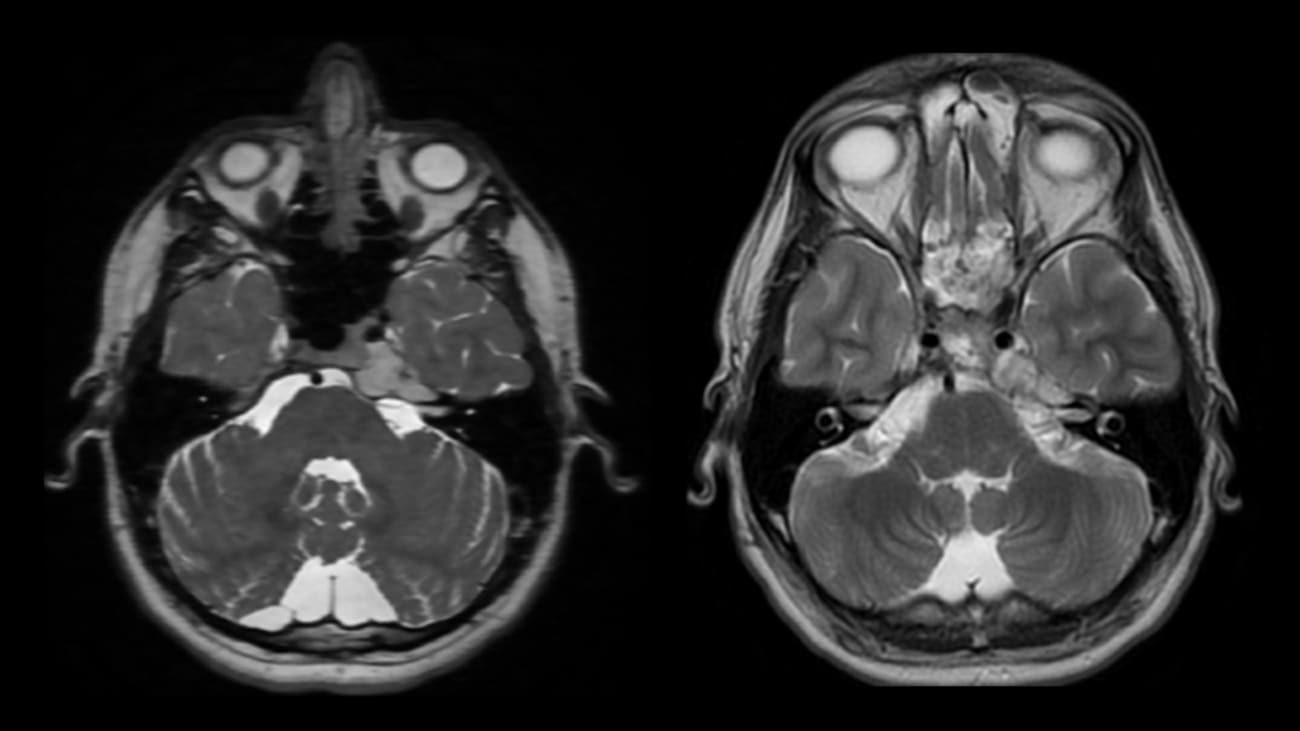
MRI showed a 4-centimeter mass in the third ventricle, with solid and cystic components abutting the bilateral anterior cerebral arteries as well as the bilateral internal carotid termini. Associated obstructive hydrocephalus with enlargement of the lateral ventricles was also seen. The patient was diagnosed with a craniopharyngioma.
“This was a large hypothalamic tumor going all the way back to the brain stem,” Goldschmidt said. “It was heavily calcified, adding to the operation’s degree of difficulty.”
Goldschmidt and Ivan H. El-Sayed, MD, UCSF otolaryngologist and head and neck surgeon, removed the tumor using the EEA. The team accomplished a near total resection, preserving the hypothalamus. “This was done to avoid hypothalamic damage, which can cause death, coma or hypothalamic obesity,” Goldschmidt said.
The patient’s symptoms subsided; she recovered well and is back with her family.
Trigeminal neuralgia relieved after resection of Meckel’s cave mass
A 43-year-old woman presented with several months of left facial pain, paresthesia and numbness. The MRI revealed a mass in the left Meckel’s cave, which was diagnosed as an epidermoid cyst. It extended from the anterior part of the skull base to the cerebellum.
“Many centers will perform a craniotomy to remove a mass in the skull base,” Goldschmidt said. “We used an endoscopic endonasal transpterygoid approach to resect this lesion.”
The procedure revealed that the trigeminal nerve was flattened by the tumor. After the UCSF team completely removed the mass, the patient no longer experienced trigeminal neuralgia. She was discharged two days later.
Patient discharged two days after chondrosarcoma removal
A 38-year-old man presented with headaches and diplopia, and his left eye was turning inward. The MRI revealed a 3-centimeter mass in the left petroclival junction, diagnosed as a chondrosarcoma.
Goldschmidt and the UCSF team removed this malignant tumor using the EEA. After the procedure, the patient’s headaches stopped, and his vision returned to normal. He was discharged in two days.
“UCSF combines clinical excellence and a rich neurosurgical tradition with modern technology and the best minds in the field,” Goldschmidt said. “It’s an environment for making new things happen, so I’m very excited to be here.”
Neurology and neurosurgery research and treatment take place within the UCSF Weill Institute for Neurosciences.
UCSF Medical Center ranks No. 1 in the nation for neurology and neurosurgery, according to the 2021-2022 Best Hospitals survey by U.S. News & World Report.
To learn more:
Phone: (415) 353-2966 | Fax: (415) 353-2167



